Pregnant Mom Has Cantaloupe-Size Tumor in Lung
UNM Emergency Teams Perform Unprecedented Surgery
Chrisela Avalos Gallegos was exhausted. She had been overjoyed to learn she was pregnant in February 2017 and was well into her second trimester as summer approached. But she couldn't understand why she felt so lethargic and couldn't shake a persistent cough.
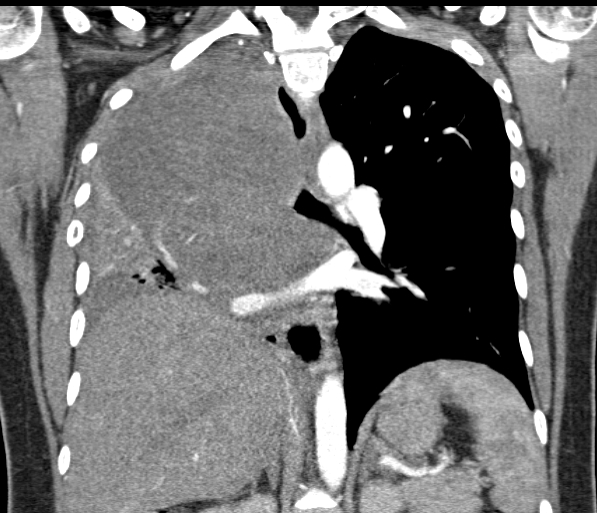
Little did she know, a cantaloupe-sized tumor had almost completely consumed her right lung and was invading the blood vessels approaching her heart. The mass was pressing on her trachea, making it difficult to breathe.
Chrisela's physicians ran select tests and everything came back normal, but she didn't feel right. Summer turned to fall and her condition only deteriorated. "It got so bad, I was really struggling to eat and keep it down," she says speaking through an interpreter.
An urgent trip to a Santa Fe emergency room in October revealed a large mass in her right lung. The hospital immediately referred Chrisela to UNM Hospital, where several expert teams were convened to plan the safe delivery of her baby. They included specialists in OB/GYN, Maternal-Fetal Medicine, High-Risk Maternal-Fetal Medicine, Extracorporeal Membrane Oxygenation, or ECMO (equipment that breathes for the patient during surgery) and Interventional Pulmonology. Also on hand were separate anesthesiology teams for mom and the baby.
As the other UNM Hospital medical teams began preparing for Chrisela's arrival, interventional pulmonologist Ali Saeed, MD, began sizing airway stents to hold these vital passageways open. A meeting between different spcialty teams determined it would be too risky to intubate Chrisela for the delivery. It was feared that she wouldn't get enough oxygen, and the baby would go into distress while in the womb.
Once the baby was delivered, Saeed knew his team would have to move in quickly to open Chrisela's airway and preserve what little breathing function she had. Saeed and his team would insert a precisely fitted stent into her trachea, the main airway, and then insert a second stent into the passageway to her functioning left lung and intubate her. Once the air passages were stabilized, he could begin working on the airway to the right lung, which was nearly filled by the tumor.
Chrisela arrived in the UNM emergency department overnight. "I was really concerned for my baby," she says. "Then I was fearful that I might not make it through surgery and see my family again."
Her initial prognosis was dire - the baby could be saved, but the teams were uncertain about Chrisela's fate. Her breathing again became labored to the point that she couldn't finish her sentences, and the teams moved in the next morning.
Approximately 70 experts filled the hospital's largest surgical suite, along with the baby's father, who scrubbed in to offer his final goodbye if Chrisela didn't survive. "We were staged in waves, with the team most needed up front and the others lined up behind," Saeed says. "When one team completed its vital work, the next rotated in, but all were aware of the mother and baby's status throughout the procedures."
Under very light sedation, Chrisela delivered a healthy, beautiful baby boy via C-section, and Saeed's team quickly went to work. "The tumor, which had all but overtaken Chrisela's right lung, had compressed her trachea flat," he says. The two stents were carefully inserted and Saeed began the first of four procedures to extract as much of the mass as possible.
"After removing a significant piece of the tumor during the second procedure, I caught a glimpse of the bottom of her right lung and felt confident we could restore its function, so we inserted a stent in her right lung," Saeed explains. "We all were so scared for her. This was an incredibly complex case requiring several delicate procedures in succession. The odds seemed against her.
"We were able to reduce the tumor to a small mass, and chemotherapy is shrinking the rest," he adds. "Our use of a multidisciplinary-team approach completely broke all barriers. We were so organized and synchronized. We really gave her the best chance we could."
How does Chrisela feel today? "It's been a slow process, but I'm certainly improving and I have this little one," she says smiling at her baby. "Walking used to take my breath away, now I can walk at a good pace and breathe fine. The only thing that takes my breath away now is Jesiah."